This post is also available in:
Your eyes are itchy, red, and troublesome. You thought that your allergies are causing flare ups, so you take antihistamines. But just when you expect to get better, your dry eye symptoms worsen. What’s going on?
Though it’s possible that you confused dry eyes with eye allergies, allergies can exacerbate dry eye symptoms as well. While the symptoms of these two conditions may appear similar, the causes and treatments are different, and they affect your body in distinctive ways. In fact, antihistamines which reduce allergy symptoms can make dry eyes worse.
Read on to understand the differences between dry eye symptoms and eye allergies.
What Causes Dry Eyes?
Dry eye syndrome is a common condition that affects 30% of Canadians—predominantly in women and older people due to changes within the body. Nevertheless, this can occur at any age, gender, and otherwise healthy people.
Dry eye condition is often caused by various reasons that disrupt the healthy tear film. Reasons around health, environment and lifestyle are many.
Some health-based reasons that could affect your ability to make tears include aging process, hormone changes, or autoimmune disease.
Some lifestyle-based reasons that might affect your tear-flow system include side effects of certain drugs like antihistamines, antidepressants, or extended use of digital devices.
Sometimes, you may experience dry eyes in certain environments that could dry out your tear film, such as on an airplane, in an air-conditioned room, or in a heater-heated room.
Symptoms for dry eyes
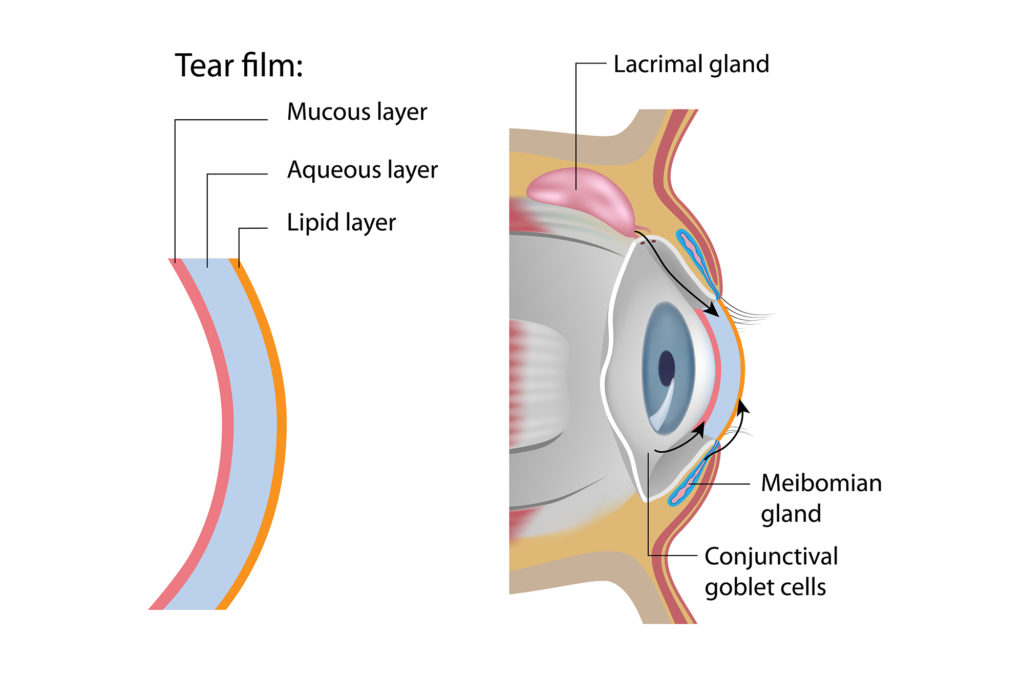
Within your tear film is three layers: fatty oils (outer), aqueous fluid (middle) and mucus (inner). Optometrist Justin Asgarpour highlights that this combination works together to ensure the surface of your eyes are lubricated, smooth and clear, “which also serves as one of the most critical components of the immune system of the eye.”
Once any of these layers is out of whack, they create multiple dry eye symptoms which vary based on the person. You may experience:
- A gritty or burning sensation
- A feeling of having something in your eyes
- Eye redness
- Sensitivity to light
- Irritation wearing contact lenses
- Watery discharge from your eyes
So, what makes a good treatment for dry eyes?
Dr. Justin Asgarpour emphasizes that “prevention is critical with dry eyes. Once you are symptomatic, the inflammatory cascade has already begun.” A good treatment for dry eyes should make you more comfortable. You’ll likely need to use multiple treatments including lifestyle changes and eyedrops to relieve and control the symptoms of dry eyes.
1. Lubrication. “Using tear drops regularly (along with other forms of treatment) ensures symptoms do not creep up,” says Dr. Asgarpour. Your eye doctor may recommend you use ointment to keep your eyes lubricated. Because it tends to make vision cloudy, as it stays in the eyes longer, it’s best used before bedtime.
2. Vitamins. A vitamin-rich diet is particularly good for your tear film. Certain vitamins such as vitamins C, E, and zinc can improve symptoms of dry eyes.
3. Anti-inflammatory nutrients. Dr. Asgarpour recommends adequate dietary intake or supplements containing omega-3 fatty acids help “reduce dry eyes related to inflammation in the Meibomian glands, allowing for less viscous oil production, and less dry eyes.” Foods that are rich in omega-3 include salmon, sardines, herring and cod. Fish oil supplements are handy if you aren’t a fish lover. Regarding plant-based foods, Dr. Asgarpour notes that “the best vegan source of EPA/DHA Omega-3 is Algae.”
4. Eyelid wipes. Lid hygiene allows for treatment of blepharitis (eyelid inflammation) which can exacerbate certain types of lipid deficient dry eyes. Use them for cleaning your lids and lashes to remove oily residue and debris. The wipes also double as a makeup remover to ensure no harmful cleaning agents enter the eye.
5. Hot compress. Heat helps unblock the Meibomian glands and make oils in your tear film runnier. Dr. Asgarpour suggests, “Soak a clean cloth in hot water—towel should be hot to the touch, but not scalding. Apply to closed eyes for about five minutes, repeating as often as needed.”
6. Blinking keeps your eyeballs moist. When you’re focused on digital screens, you blink less, and your upper eyelid doesn’t shut completely. It may be helpful to regularly close your eyes for a few minutes or blink repeatedly for a few seconds to help spread your tears evenly over your eyes.
What causes eye allergies?
Allergy reactions occur when your body responds to the exposure of a substance from the environment or food. Your immune system releases histamine to defend against these substances that seem foreign to the body.
The most common type of eye allergy is seasonal. When a susceptible person experiences more ocular allergy symptoms in the spring and fall, they may be allergic to pollens.
If you experience symptoms year-round, then you may be allergic to other allergens, such as pet dander, smoke or dust mites.
The risk of eye allergy gets higher if you have nasal allergies or hay fever.

Eye allergy: Treatment and prevention
Though the best way to avoid allergies is to prevent your exposure to substances that trigger your allergy, this isn’t always possible. You’ll likely need to be prepared to handle them.
1. Antihistamines. Prescribed to relieve allergy symptoms such as the itch and rash caused by the release of histamine in your body. It’s important to seek care from your eye care professional to receive the best medication.
2. Allergy drops. Prescribed to soothe eye allergy symptoms almost instantly. Consider the following eye allergy products: Soothe Allergy Eye Drop and Opti Tears Allergy Drop. It’s imperative to seek guidance for your eye doctor to get the best medication.
3. Lid wipes. Help alleviate your discomfort and maintain hygiene simultaneously. Avoid rubbing or touching your eyes during an allergy flare-up, as both habits can spread germs and cause more irritation.
4. Cold compress. Cold temperatures can have a soothing effect on your eyes by reducing inflammation, thereby minimizing the itch, swelling, and redness. Soak a clean cloth in cold water and apply to closed eyes.
Takeaway: Dry eyes and allergies
We hope that we’ve helped you understand the differences between dry eye symptoms and eye allergies. If it’s tricky to tell them apart, see your doctor to get the right diagnosis and treatment.